Today begins with me being enlightened about how coming from the country means I am naturally incestuous with six fingers. I can confirm that this is not true.
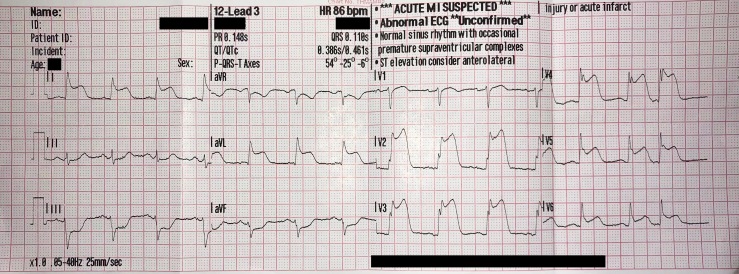
We’re dispatched almost immediately to a patient in their fifties with cardiac chest pain. On arrival, they’re laid on the pavement breathing at 76 a minute and are in quite evident distress. We don’t dilly dally around. The patient is in the back of the ambulance within minutes. I do a 12-lead ECG (a tracing of the hearts electrical activity, pictured below). The tracing confirms that the patient is having a rather significant heart attack or MI (myocardial infarction in fancy medical talk). Aspirin, clopidogrel and GTN are given, as standard, and I alert the PPCI (primary percutaneous coronary intervention) department, which is only the best part of a 50-minute drive (on blue lights). The monitor then shows my patient is in cardiac arrest. I promptly alert my colleagues. Compressions are started immediately and he is shocked twice – we achieve ROSC (return of spontaneous circulation – basically we’ve brought the patient back to life). Although by now, the patient has technically died and been resuscitated, all they keep saying is how they’re going in and out of consciousness. I think we did quite a good job. The patient is stable for the rest of the journey to the PPCI. I am allowed to watch the angioplasty, which is successful.*
Naturally, the rest of the day was fairly mundane after this bout of excitement.±
* Angioplasty carries significant risks. For example, the embolus causing occlusion in the heart can, once dislodged, travel to the brain and cause a massive stroke.
± Is that a little sadistic?
